by Claire Taylor
98%
of PrEP recipients have ever attended clinic
353,173
unique SHL service users ordered ≥1 STI test kits during the study period
6%
service users taking PrEP were still self-sourcing it
Dr Sara Day, Sophie Jones, Efejiro Ashano, Will Nutland, Jonathan Spate, Laura Stewart.
Background
In England, PrEP was nationally commissioned in October 2020. Prior to this, unless individuals wishing to take PrEP were recruited to research studies, they needed to self-source or self-pay for medication online. We identified the number and characteristics of individuals accessing SHL, London’s online postal STI testing service, that reported self-sourcing PrEP after it became available on the National Health Service (NHS).
Method
When ordering a SHL test kit service users complete an e-questionnaire which captures current PrEP use and where PrEP is obtained. The e-notes of individuals disclosing PrEP use between 1/2/21–1/10/22 were reviewed. Demographics, PrEP source, prior attendance to sexual health clinic (SHC) and STI rates were collected.
Results
353,173 unique SHL service users ordered ≥1 STI test kits during the study period and 20,365/353,173 (5.8%) reported taking PrEP on their e-questionnaire. 18086/20365 (88.8%) users sourced PrEP from a SHC, 1615 (7.9%)
self-sourced it and 664 (3.3%) provided no source details.
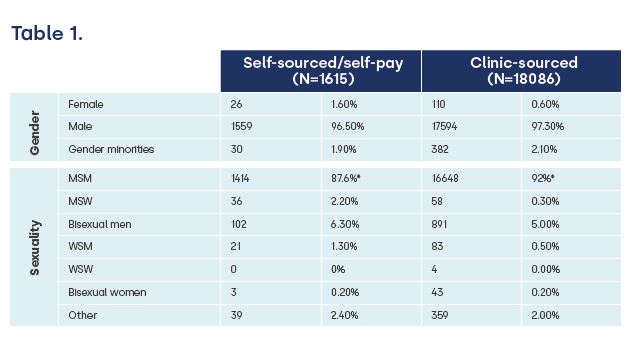
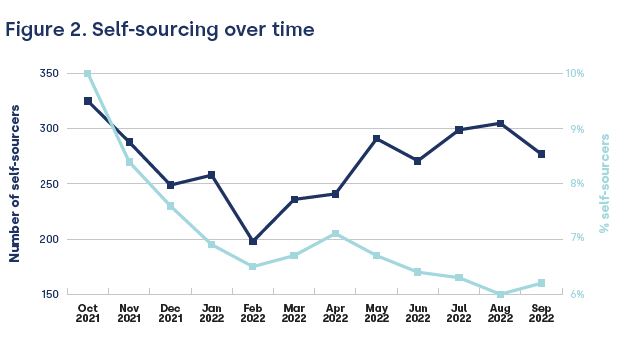
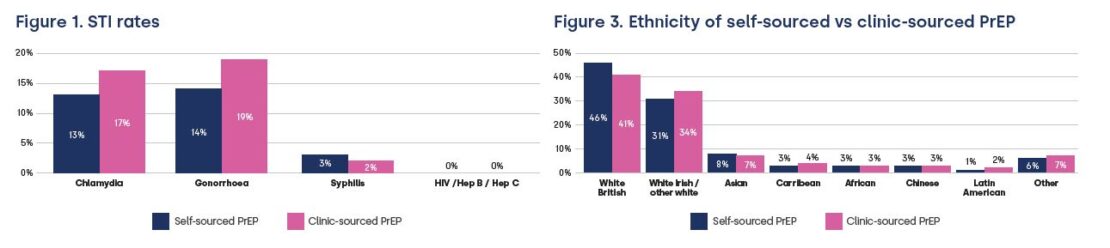
18015 (88.5%) users reported SHC attendance (for any reason) within the previous 12m, 1912 (9.4%) attended more than a year ago and 438 (2.2%) had never attended clinic. Gender and sexuality of PrEP users is shown in Table 1. STI rates, change in self-sourcing over time, and ethnicity are shown in Figures 1–3.
Conclusion
It is reassuring 98% PrEP recipients have ever attended clinic where access to additional important interventions such as vaccinations, renal monitoring, checking adherence/compliance and risk reduction support are available. Despite this, in September 2022, over 6% service users taking PrEP were still self-sourcing it despite its availability within the NHS. This may be due to difficulties accessing clinic/PrEP services, lack of awareness of its NHS availability, ineligibility for NHS PrEP or personal preference.
The volume and proportions self-sourcing PrEP are declining over time whilst clinics recover from the pandemic and adapting to meet demand, but improvements in public awareness and removing barriers to accessing clinic/PrEP services, especially in underrepresented (non-MSM) groups are warranted. Staff training in PrEP eligibility, and use of practices that reduce bias (eg. gender bias) and disparity in access are required. Making access easier eg. online booking and offering wider variety of appointments could be considered, including more evening/weekend or virtual consultations.



About the author:
Claire is the Senior Digital Marketing Executive at Preventx.